Definition and epidemiology
• Ulcer is defined as a large tissue defect that goes beyond the muscularis mucosa to the submucosa and deeper layers in the GIS. Erosion is a defect in the superficial mucosa only.
• Ulcers seen in the upper GIS are defined as peptic ulcers because of their relationship with acid and pepsin.
• Duodenal ulcers are mostly located on the anterior wall of the bulb, gastric ulcers are mostly located on the antrum and incisura angularis.
• Duodenal ulcer is seen approximately 3 times more frequently than gastric ulcer.
Etiology and Pathogenesis
• Ulcer; It is caused by the deterioration of the balance between protective factors and aggressive factors for the gastric and duodenal mucosa.
• It is more important to decrease the protective factors in the formation of gastric ulcer and to increase the aggressive factors in the formation of duodenal ulcer.
• Today, the most important aggressive factor is H. pylori.
• Duodenal ulcers are usually associated with hyperacidity, gastric ulcers usually with normo- or hypoacidity.
• Factors that provide mucosal continuity (protective factors)
mucus layer
Bicarbonate
Mucosal blood flow
cell regeneration
Endogenous prostaglandins
nitric oxide
• Aggressive factors that increase the risk of ulcers
H. pylori (associated with 70% of duodenal ulcers, 50% of gastric ulcers)
NSAID / aspirin
Cigaret
Stress
Increase in acid secretion (gastrinoma, mastocytosis, basophilia, hyperparathyroidism etc.)
• Other: Many chronic systemic diseases (COPD, CKD, diabetes, etc.), alcohol, O blood group and advanced age are other factors that increase the risk of ulcers.
• The role of diet in the pathogenesis of ulcer has not been demonstrated. However, in someone with an ulcer, certain foods may increase symptoms.
• Although smoking is an aggressive factor, it also reduces protective factors. Therefore, peptic ulcer heals more difficult in smokers and relapses more frequently.
• NSAIDs cause mucosal erosion and ulcers as a result of both local toxic effects (direct) and systemic effects (indirect).
NSAIDs reduce prostaglandin synthesis (systemic effect), disrupt mucosal blood flow and barrier, decrease bicarbonate and mucus synthesis.
NSAIDs show their effects by inhibiting the cyclooxygenase (COX) enzyme. This enzyme has COX-1 and COX-2 subtypes. COX-1 inhibition is more important in the formation of GIS side effects, and COX-2 inhibition in the formation of anti-inflammatory effects.
Gastric erosion and ulcers are rarer with drugs that selectively inhibit COX-2. However, cardiac side effects can also be seen with these drugs.
• Conditions that increase the risk of GI complications in patients taking NSAIDs;
Previous ulcer bleeding (most important risk)
Age (over 65)
History of peptic ulcer
high dose NSAID
Multiple NSAIDs
Combined aspirin or steroid intake
Concomitant use of anticoagulant drugs
Concomitant systemic disease(s)
• Long-term PPI prophylaxis is recommended in patients with multiple risk factors or with previous ulcer bleeding. Misoprostol can also be used for prophylaxis.
• The most effective approach to prevent NSAID-related gastroduodenal damage is the combination of PPI and selective COX-2 inhibitors.
Clinic
• Patients often present with dyspeptic complaints. Abdominal pain is most common.
• Ulcer pain is periodic (frequent in spring and autumn), repetitive, relieved by food and antacid, increased by hunger, and awakened at night. Night awakening pain is the most valuable symptom, especially for duodenal ulcer.
• Symptoms usually begin two hours after meals in duodenal ulcers, and earlier in gastric ulcers.
• The character of the pain can also guide the complications of peptic ulcer.
Diagnosis
• Endoscopy is the most valuable and first-choice diagnostic method, and it also allows biopsy from the lesion.
• In all gastric ulcers, biopsy should be taken to exclude malignancy, and even if the pathology result is reported as benign, endoscopy should be repeated 1-2 months later to check whether the ulcer heals or not. (Stomach ulcer does not turn into cancer, but stomach cancer may look like an ulcer)
• Duodenal ulcer, on the other hand, does not require biopsy and endoscopic follow-up, because the frequency of cancer in this region and therefore the probability of mixing the cancer with the ulcer is very low.
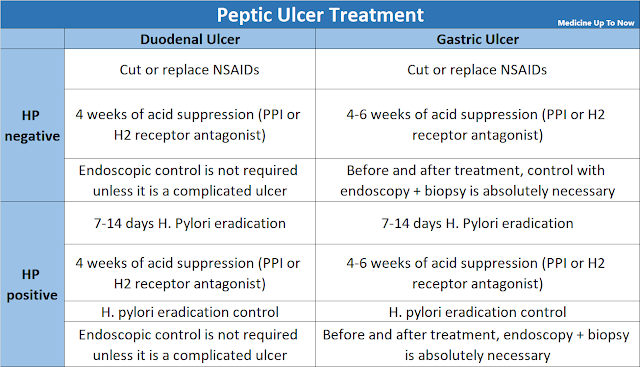
Treatment
• Diet: The effect of diet in ulcer treatment has not been demonstrated. Patients are advised to avoid foods that only increase their symptoms.
• Refractory ulcer: Ulcers that do not heal within 8-12 weeks despite pharmacological treatment are considered refractory.Malignancy should be excluded in refractory gastric ulcers.
In addition, all refractory ulcers should be investigated for gastrinoma and other systemic diseases with hyperacidity.
• Surgical treatment: It is performed in cases that are refractory to all medical treatments or for complications.
Peptic Ulcer Complications
• Bleeding
It is the most common complication.
Peptic ulcer is the most common cause of upper GI bleeding.
Bulbus posterior wall ulcers are more frequent and prone to profuse bleeding.
• Perforation
It is the second most common complication after bleeding.
It is more common in ulcers on the anterior duodenal wall and gastric lesser curvature.
Severe and sudden pain should suggest perforation.
It is the most common indication for emergency surgery.
• Penetration
In duodenal ulcers, it most often occurs to the pancreas. Gastric ulcers penetrate the left hepatic lobe.
The fact that the pain hits the lower back and the right upper quadrant, is not relieved by antacids, but is continuous, suggests penetration.
• Obstruction
It most commonly occurs in pyloric duct ulcers.
Pain that increases with meals and is accompanied by nausea and vomiting should suggest gastric outlet obstruction.